This CME is presented in loving memory of Susan M. (White) Kelemen, July 4, 1939 – February 26, 2022, by her family, the Montecalvos and the Kelemens.
Instructor
Monica E. Embers, PhD
Associate Professor in the Division of Immunology
Director of Vector-borne Disease Research
Tulane National Primate Research Center
Description
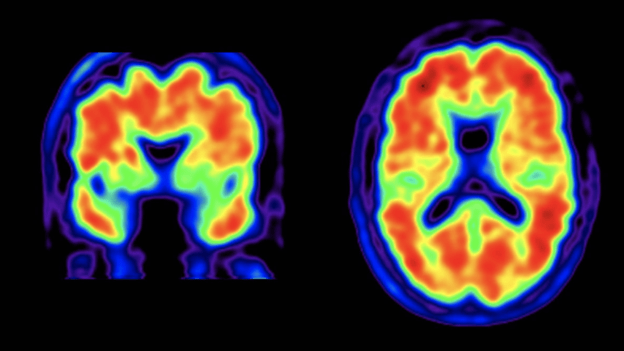
This module describes the features of dementia and microbes which have been implicated in the development of this type of neurological disease. The gaps in knowledge regarding the development of dementia are highlighted. Finally, a case report from a patient who developed Lewy body dementia following a Lyme disease diagnosis is discussed.
Learning objectives
- To review the prevalence and different types of dementia
- To describe the clinical and pathological features of dementia
- To consider the possible mechanisms of neurological damage (that are consistent with dementia pathology) induced by microbes
- To define the gaps in knowledge regarding the etiology of Alzheimer’s and Lewy body dementia• To provide evidence for the probable role of the Lyme disease spirochete in dementia etiology several years after unsuccessful treatment for Lyme disease (case report).
This session, Chronic infection and the etiology of dementia, is approved for 0.5 enduring AAFP Prescribed credits.
AAFP Prescribed credit is accepted by the American Medical Association as equivalent to AMA PRA Category 1 credit(s)™ toward the AMA Physician’s Recognition Award. When applying for the AMA PRA, Prescribed credit earned must be reported as Prescribed, not as Category 1.
The AAFP has reviewed One Health Medical Education for a Changing Climate and deemed it acceptable for AAFP credit. Term of approval is from 01/02/2024 to 01/01/2025. Physicians should claim only the credit commensurate with the extent of their participation in the activity.
References
Embers ME, Hasenkampf NR, Jacobs MB, Tardo AC, Doyle-Meyers LA, Philipp MT, Hodzic E: Variable manifestations, diverse seroreactivity and post-treatment persistence in non-human primates exposed to Borrelia burgdorferi by tick feeding. PLoS ONE 2017, 12(12):e0189071.
Crossland NA, Alvarez X, Embers ME: Late Disseminated Lyme Disease: Associated Pathology and Spirochete Persistence Posttreatment in Rhesus Macaques. The American Journal of Pathology 2018, 188(3):672-682
A.B. MacDonald: Plaques of Alzheimer’s disease originate from cysts of Borrelia burgdorferi, the Lyme disease spirochete. Med Hypotheses, 67 (2006), pp. 592-600
Amor S, Puentes F, Baker D, Valk vd, P. Inflammation in neurodegenerative diseases. Immunology. 2010;129(2):154-169. https://www.narcis.nl/publication/RecordID/vu2:oai:dare.ubvu.vu.nl:1871%2F45580. doi: 10.1111/j.1365-2567.2009.03225.x.
Serrano-Pozo A, Frosch MP, Masliah E, Hyman BT. Neuropathological alterations in alzheimer disease. Cold Spring Harbor perspectives in medicine. 2011;1(1):a006189. https://www.ncbi.nlm.nih.gov/pubmed/22229116. doi: 10.1101/cshperspect.a006189.
Qiu C, Kivipelto M, von Strauss E. Epidemiology of alzheimer’s disease: Occurrence, determinants, and strategies toward intervention.
Dialogues in clinical neuroscience. 2009;11(2):111-128. https://www.ncbi.nlm.nih.gov/pubmed/19585947.
Raber J, Huang Y, Ashford JW. ApoE genotype accounts for the vast majority of AD risk and AD pathology. Neurobiology of Aging. 2004;25(5):641-650. https://www.sciencedirect.com/science/article/pii/S0197458004001009. doi: 10.1016/j.neurobiolaging.2003.12.023
Itzhaki RF, Lin W, Shang D, Wilcock GK, Faragher B, Jamieson GA. Herpes simplex virus type 1 in brain and risk of alzheimer’s disease. The Lancet. 1997;349(9047):241-244. https://www.sciencedirect.com/science/article/pii/S0140673696101495. doi: 10.1016/S0140- 6736(96)10149-5.
Itzhaki RF. Herpes simplex virus type 1 and alzheimer’s disease: Increasing evidence for a major role of the virus. Frontiers in aging neuroscience. 2014;6:202. https://www.ncbi.nlm.nih.gov/pubmed/25157230. doi: 10.3389/fnagi.2014.00202.
Itzhaki RF. Herpes simplex virus type 1 and Alzheimer’s disease: Possible mechanisms and signposts. FASEB journal : official publication of the Federation of American Societies for Experimental Biology. 2017;31(8):3216. https://www.ncbi.nlm.nih.gov/pubmed/28765170.
Mawanda F, Wallace R: Can Infections Cause Alzheimer’s Disease? Epidemiologic Reviews 2013, 35(1):161-180.
Soscia SJ, Kirby JE, Washicosky KJ, Tucker SM, Ingelsson M, Hyman B, Burton MA, Goldstein LE, Duong S, Tanzi RE et al: The Alzheimer’s disease-associated amyloid beta-protein is an antimicrobial peptide. PLoS ONE 2010, 5(3):0009505.
Miklossy J: Bacterial Amyloid and DNA are Important Constituents of Senile Plaques: Further Evidence of the Spirochetal and Biofilm Nature of Senile Plaques. J Alzheimers Dis 2016, 53(4):1459-1473.
Gadila, S. K. G., Rosoklija, G., Dwork, A. J., Fallon, B. A., & Embers, M. E. (2021). Detecting Borrelia Spirochetes: A Case Study With Validation Among Autopsy Specimens. Front Neurol, 12, 628045. https://doi.org/10.3389/fneur.2021.628045
Balin BJ, Hammond CJ, Little CS, et al. Chlamydia pneumoniae: An Etiologic Agent for Late-Onset Dementia. Front Aging Neurosci. 2018;10:302. Published 2018 Oct 9. doi:10.3389/fnagi.2018.0030216. Gérard HC, Dreses-Werringloer U, Wildt KS, Deka S, Oszust C, Balin BJ, Frey WH 2nd, Bordayo EZ, Whittum-Hudson JA, Hudson AP. Chlamydophila (Chlamydia) pneumoniae in the Alzheimer’s brain. FEMS Immunol Med Microbiol. 2006):355-66. doi: 10.1111/j.1574-695X.2006.00154.x. Epub 2006 Oct 18. PMID: 17052268.